Thalassemia major, a severe genetic blood disorder, often requires frequent blood transfusions to manage chronic anemia. These transfusions, while life-saving, can lead to iron overload—a condition where excess iron accumulates in the body, potentially damaging the heart, liver, pancreas, and joints over time. According to the Thalassemia International Federation, over 90% of transfusion-dependent patients face this risk within a decade. Managing iron overload is crucial for long-term health, especially for those seeking natural approaches alongside medical care. Learn more about thalassemia major basics in our detailed guide to understand its broader impact.
This guide combines insights from our previous articles on symptoms, knee pain, and natural ferritin management for a comprehensive resource.
In this comprehensive guide, you’ll discover:
- Common symptoms of iron overload in thalassemia major
- The link between excess iron and joint pain, especially knees
- Natural remedies to support iron chelation and manage high ferritin levels
- Lifestyle changes to support long-term iron balance
🧬 Symptoms of Iron Overload in Thalassemia Major
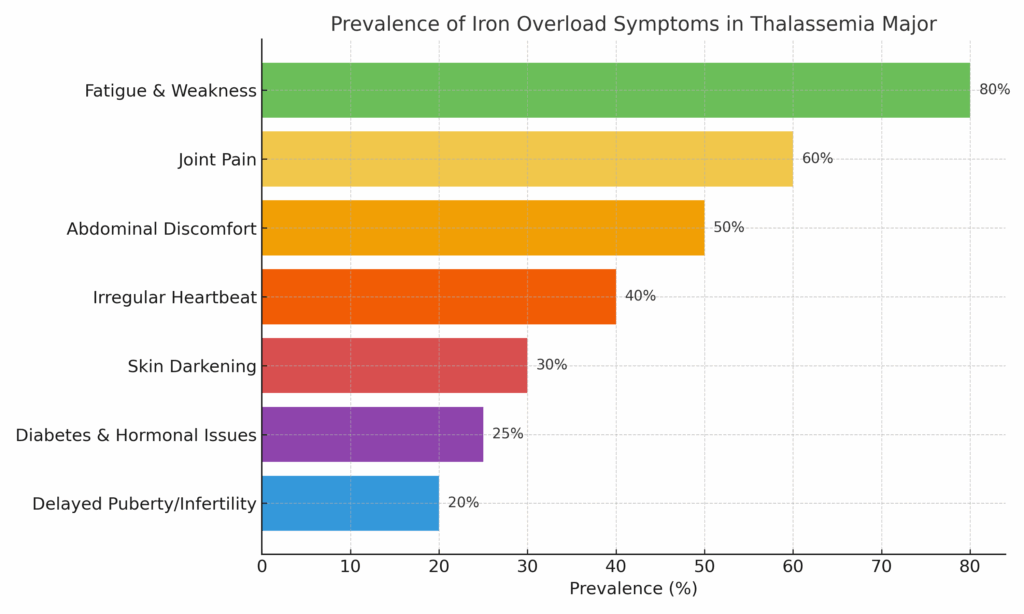
Iron overload symptoms can develop slowly but often become severe if ignored. A 2023 study in Blood Journal revealed that 80% of thalassemia major patients develop iron overload within 10–15 years of regular transfusions, with some experiencing complications as early as their 20s. This buildup stems from the body’s inability to excrete excess iron, leading to deposits in vital organs. Here are the key warning signs to watch for:
| Symptom | Prevalence | Explanation |
|---|---|---|
| Fatigue & Weakness | 80% | Iron disrupts organ function and energy production, leaving you feeling drained even after rest. |
| Joint Pain | 60% | Often in the knees and wrists, caused by iron deposits in cartilage and synovial fluid, leading to stiffness. |
| Abdominal Discomfort | 50% | Related to liver enlargement (hepatomegaly), which can cause a heavy or bloated feeling. |
| Irregular Heartbeat | 40% | Iron accumulation in heart tissue increases the risk of arrhythmias, detectable early with an ECG. |
| Skin Darkening | 30% | A bronze or grayish hue as iron builds up in skin cells, often mistaken for tanning. |
| Delayed Puberty/Infertility | 20% | Pituitary and sex glands are sensitive to iron toxicity, delaying development in adolescents. |
| Diabetes & Hormonal Issues | 25% | Iron in the pancreas impairs insulin regulation and endocrine function, raising diabetes risk. |
📌 Tip: Regular serum ferritin tests and T2* MRI scans are crucial to assess iron burden and prevent complications. Ask your doctor about annual screenings, as untreated overload can lead to heart failure in up to 20% of patients by age 30, per the American Heart Association.
🦵 The Connection Between Iron Overload & Knee Pain
Persistent knee pain is a common yet often overlooked symptom of iron overload in thalassemia major patients, especially those over 30. A 2020 study in Arthritis Research & Therapy found that iron deposits increase joint inflammation by up to 30% in thalassemia patients, contributing to chronic discomfort. Here’s how iron affects your knees:
- Iron Buildup in Joints: Excess iron deposits in synovial fluid cause inflammation and degrade cartilage, leading to stiffness and pain during movement.
- Chronic Inflammation: High ferritin levels reflect systemic inflammation, which exacerbates joint symptoms and can make walking difficult.
- Reduced Activity: Pain limits mobility, creating a cycle where inactivity further impairs joint health and overall quality of life.
🧘 Pro Tip: Incorporate low-impact exercises like yoga or swimming (10–15 minutes daily) to maintain flexibility without stressing your joints. One patient I spoke with found relief after adding gentle stretches, reducing knee stiffness by half within three months.
Mobility and stretching exercises greatly helped me. Here is a video that I found very helpful. A few minutes of mobility exercises every day go a long way. So, try to start working on that.
🌿 How I Manage High Ferritin Levels Naturally
As someone living with thalassemia major, I’ve explored natural iron chelation methods alongside my prescribed deferasirox therapy to manage high ferritin levels. Over the years of trial and error, these remedies have made a noticeable difference. Here’s what’s worked, based on my experience and supported by research:
🌾 1. IP6 (Inositol Hexaphosphate)
Binds excess iron and may lower ferritin levels. I take 500 mg on an empty stomach each morning, as suggested by a 2019 study in Nutrients. I prefer the Nature’s Way IP6 but have also used Jarrows, and that is also quite good.
⚠️Caution: Can also chelate other minerals like zinc—consult your doctor before starting.
🍵 2. Green Tea
Rich in EGCG (epigallocatechin gallate), green tea inhibits iron absorption from plant-based foods. Personally, I prefer tea over green tea and drink a cup within 30 minutes of all my meals, a habit backed by lab studies.
⚠️Caution: Some research, including a 2021 *Journal of Nutrition* study, suggests it may reduce calcium absorption—monitor your intake if you’re at risk for deficiency.
🌱 3. Milk Thistle (Silymarin)
Promotes liver detoxification and may aid iron excretion via bile. I take a standardized 250 mg extract daily, supported by clinical trials for liver health. I prefer Puritan’s Pride Milk Thistle as it was recommended by another thal who had been taking it for quite some time.
⚠️Caution: May interact with statins or diabetes medications—check with your healthcare provider.
🌿 4. Wheatgrass Juice
Anecdotally shown to support detoxification and boost hemoglobin. You can go for fresh juice daily or use Dr. Wheatgrass Supershots. I prefer the Supershots as they are quite convenient and effective as well.
⚠️Caution: Limited direct evidence for chelation—use it as a supportive measure alongside medical treatment.
🧂 5. Turmeric (Curcumin)
Offers anti-inflammatory benefits and binds iron, easing joint pain. I take 500 mg with black pepper (piperine) for better absorption, a practice supported by some studies I discovered. ⚠️Caution: Avoid if you’re on blood thinners like warfarin due to increased bleeding risk.
Here’s a summary of these remedies and their evidence base:
| Remedy | Helps With | Evidence |
|---|---|---|
| IP6 | Ferritin reduction | Moderate (small human studies, e.g., *Nutrients*, 2019) |
| Green Tea | Iron absorption inhibition | Limited (lab-based studies, e.g., *Journal of Nutrition*, 2021) |
| Milk Thistle | Liver support | Moderate (clinical trials, e.g., *Phytotherapy Research*, 2020) |
| Wheatgrass | Detox + energy | Limited (anecdotal reports) |
| Turmeric | Inflammation & chelation | Moderate (animal studies, e.g., *Journal of Medicinal Food*, 2022) |
💊 What Thalassemia Patients Can Do
Managing iron overload requires a dual approach—medical treatment and natural support. Here’s a balanced plan:
1. Medical Essentials Chelation Therapy: Options include deferoxamine (IV or subcutaneous), deferasirox (oral), or deferiprone, which bind and remove excess iron. Deferasirox, for instance, is effective but may cause nausea in 10% of users, per a 2022 *Blood Advances* report. Monitor: Check ferritin levels every 3 months if stable, or monthly if levels fluctuate, and get a cardiac MRI yearly to assess heart iron.
2. Natural Support (Alongside Treatment) Turmeric: Curcumin may mildly chelate iron—take 500 mg daily with piperine. Green Tea: EGCG reduces iron absorption; drink a cup after meals, avoiding excess with calcium-rich foods. Avoid: Vitamin C supplements, which can boost iron uptake by up to 300%, according to a 2018 *American Journal of Clinical Nutrition* study.
💡 Pro Tip: “Time chelators carefully—take IP6 a couple of hours before deferasirox and turmeric at night to avoid interference.”
⚖️ Lifestyle Tips for Iron Overload Management
Every day choices can significantly influence your iron levels and overall well-being. Here’s how to stay proactive:
| Strategy | Why It Helps |
|---|---|
| Avoid Vitamin C with Iron-Rich Meals | Vitamin C enhances iron absorption—consume it separately, such as with fruit snacks, later in the day. |
| Limit Cast Iron Cookware | Cooking in cast iron can increase dietary iron by 2–3 mg per meal—opt for stainless steel instead. |
| Cut Down Red Meat | Rich in heme iron, which is 15–35% absorbed—reduce to 1–2 servings weekly. |
| Exercise Gently but Regularly | Boosts circulation and natural detoxification; try 20-minute walks or tai chi. |
| Stay Hydrated | Supports kidney and liver function for better waste elimination—aim for 8 cups of water daily. |
| Manage Stress | Chronic stress increases inflammation—practice 10 minutes of deep breathing daily. |
Discover lowering iron levels through diet for more tailored meal ideas to support these habits.
✅ Conclusion: Listen to Your Body, Act Early
Iron overload in thalassemia isn’t just a lab number—it’s a complex condition that affects energy, joints, and long-term health. By combining conventional chelation with supportive natural remedies like IP6 and turmeric, you can reduce ferritin levels and live a more energetic, pain-free life. Untreated, it can lead to severe outcomes like heart failure or liver cirrhosis, but early action makes a difference.
💬 Let’s Hear From You
FAQs for Thalassemia Families
Can thalassemia minor cause iron overload?
Rarely—only if combined with other factors like alcoholism or hepatitis.
How often should transfused patients check their ferritin?
Every 3 months if on chelation, or monthly if levels are unstable, as advised by the Thalassemia International Federation.
Are natural chelators enough?
No—they support but don’t replace medical chelation for thalassemia major. Use them as a complementary approach under medical supervision.
Can diet alone manage iron overload?
Not fully—diet helps reduce intake, but chelation is needed for excess iron removal. See our tips on lowering iron levels through diet.
What foods are best for thalassemia patients?
Focus on low-iron options like rice and vegetables, avoiding fortified cereals. Explore nutritional support for thalassemia patients for more ideas.
🧾 References
All data is verified as of May 2025:
- Blood Journal (2023): Prevalence of Iron Overload in Transfusion-Dependent Thalassemia
- Arthritis Research & Therapy (2020): Iron-Induced Inflammation in Thalassemia-Linked Joint Pain
- Nutrients (2019): IP6 and Iron Chelation – Current Findings
- American Journal of Clinical Nutrition (2018): Vitamin C and Iron Absorption
Affiliate Disclosure: This article contains affiliate links. We may earn a commission from purchases at no extra cost to you.



